Snoring is often dismissed as an annoying or unfortunate fluke in your sleep habits. However, it can also be a sign of something much more serious—a sleep disorder. The American Academy of Sleep Medicine estimates that 50-70 million U.S. adults suffer from some form of sleep disorder.
The most common sleep disorder is sleep apnea, which affects 25 million adults in the U.S. An apnea, or temporary pause in breathing, is in many cases caused by the tissue in the back of the throat collapsing during sleep. Other sleep disorders that can be diagnosed from a sleep study include parasomnia (sleepwalking), sleep eating, nocturnal seizures, unexplainable insomnia, poor sleep and narcolepsy.
Sleep disorders can cause annoying symptoms like the inability to fall or stay asleep or a feeling of drowsiness throughout the day. In the short term, that condition could cause you to get into an accident, but there are also potential long-term effects on your health.
Recognizing and diagnosing sleep disorders
When a sleep disorder is suspected by your doctor, they may order a sleep study to be performed in your home or in a sleep lab. “Most patients report to clinic with insomnia, or trouble falling or staying asleep,” says Dr. Suhaib Haq, family medicine physician and sleep medicine specialist at University Health. “The other complaint they present with is that they are very sleepy. Most of the time, people put up with these conditions for years before seeking help.”
Dr. Haq warns that ignoring the signs of a sleep disorder can have severe consequences on your health. “The most immediate and potentially fatal outcome of a sleep condition is becoming sleepy behind the wheel and causing an accident,” he says. “Drowsy driving is responsible for 1,500 fatalities and up to 40,000 non-fatal injuries every year.”
There are also long-term negative effects of ignoring a sleep condition, including:
- diabetes
- high blood pressure
- depression
- pain
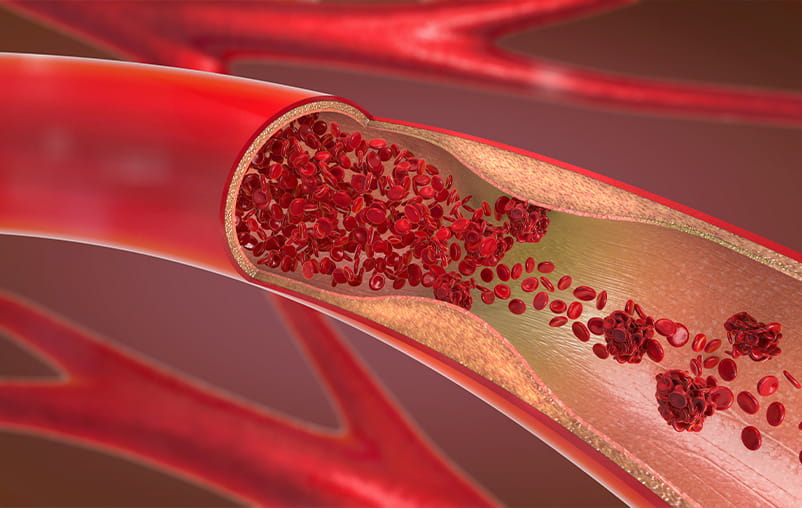
- heart problems
- stroke
“Sleep is when we rest, restore and rejuvenate our body,” says Dr. Haq. “When somebody has poor sleep, their risk for these chronic conditions is greater. The long-term effects can be drastic if a sleep concern is not addressed properly.”
According to Dr. Haq, you are at higher risk for a sleep disorder if you notice snoring, especially when combined with any of these factors:
- body mass index (BMI) higher than 25
- high blood pressure
- family history
- neck size of 17 inches or more for men
- neck size of 16 inches of more for women
Men are also at a higher risk than women, as are people over 40.
If you notice any of the warning signs of a sleep disorder and/or have any of these risk factors, your doctor may order a sleep study to be performed on you to learn more.
What happens during a sleep study?
There are two types of sleep studies: those conducted in the comfort of your home, and studies performed in a controlled sleep lab. In a home sleep study, you are outfitted with sensors that measure your breathing, movement, and sometimes brain waves. Patients take the equipment home and return it after the study to have the results analyzed.
“Home sleep studies are great for a patient’s comfort, but a home-based study can only be used to diagnose sleep apnea,” says Dr. Haq. “It cannot identify other disorders that can be identified through a study in the sleep lab.”
A study conducted in the sleep lab involves more types of sensors and round-the-clock monitoring by trained technicians.
Sleep studies in a lab can measure a patient’s brain waves, oxygen levels and heart rhythm and rate. Patients are also outfitted with a microphone to record snoring or teeth grinding and an abdomen belt that measures breathing movement. There are also sensors on the hands and feet that can measure movement of the limbs to diagnose a sleep condition called periodic limb movement disorder and sensors on the eyes to measure eye movement.
How do doctors process and analyze all of that information? “The system is very efficient,” says Dr. Haq. “When a patient is being studied, the techs are measuring and recording findings throughout the night. By the morning the data has been collected, processed and analyzed in real-time. The doctor gets the report to analyze the information without unnecessary distractions, but the whole process takes a village to complete.”
The process is also recorded, and if technicians find signs of moderate to severe sleep apnea they can intervene and put the patient on a breathing device right away.
How are sleep disorders treated?
Continuous positive airway pressure (CPAP) therapy is the most common treatment for sleep apnea, which accounts for around 70% of all diagnosed sleep disorders. CPAP machines provide a constant stream of air through a face mask, eliminating breathing pauses and snoring or choking noises.
If you are diagnosed with sleep apnea, your doctor will likely prescribe CPAP therapy for you to eliminate the gaps in your breathing and help you get a good night’s rest.
COVID-19 and sleep studies
Many patients are understandably nervous about the idea of undergoing a sleep study during the COVID-19 pandemic. Dr. Haq says there is little risk to engaging in a study. “Our sleep labs follow the standard set by the American Academy of Sleep Medicine,” he says. “We follow all hygiene and distancing protocols, and all patients are screened for COVID-19 before they come for the test.”
There is also comprehensive staff testing, masks are required at all times, and all equipment is cleaned and sanitized to the highest standards and recommendations.
“I would go and get a sleep test done without any hesitation,” says Dr. Haq. “It is a safe place to be—safer than a restaurant, a store or a car dealership. We take patient safety as our utmost priority and do everything possible to keep the environment clean and safe.”
Patients are concerned about COVID-19 and CPAP
Because CPAP machines produce positive pressure, they recirculate particles from a person’s breath into the air. “Patients have asked us if it is safe to use their equipment if they or someone in their household has COVID-19,” says Dr. Haq. They are concerned they might spread the virus to others. “Sleep machines like CPAP do present a risk of disseminating the virus into the air because they express positive pressure,” he says.
Dr. Haq recommends patients who use a CPAP machine and test positive for COVID-19 should stay in complete isolation so they can continue to use their machines. “It’s important that no one else goes into their room,” he says, “especially when they are using their machine.”
The silent killer
“COVID-19 itself has brought up and unmasked underlying anxiety and depression in a lot of patients and staff,” says Dr. Haq. “That’s across the board, including patients who already have sleep-related disorders.”
Anxiety and depression negatively affect people’s sleep and sleep hygiene, and sleep disorders are not a condition to take lightly. They are often ignored or go unnoticed because the condition occurs at night, but the consequences of ignoring a sleep disorder can be deadly.
“Sleep apnea is the real silent killer,” says Dr. Haq. “Untreated, it can make your life miserable. You wake up tired, and stay sleepy throughout the day, but it can also affect your heart, lungs, memory process and could cause a fatal car accident.”
Symptoms like snoring and drowsiness coupled with the common risk factors for a sleep disorder should not be ignored. If you think you’re at risk, Dr. Haq has a very clear recommendation. “If you’re snoring and you have the risk factors, don’t wait,” he says. “Talk to your doctor and see if you need to be checked for sleep apnea.”